Cardiovascular disease remains a leading cause of premature death in the United States, with concerning disparities across different regions and socioeconomic groups. A recent study has shed light on this alarming trend, revealing a strong association between county-level social deprivation and premature mortality related to a condition known as cardio-kidney-metabolic (CKM) syndrome.
arterydisease’>coronary artery disease, failure’>heart failure. The CKM syndrome, as defined by the American Heart Association, represents the intersection of metabolic, renal, and cardiovascular conditions, which together contribute to a significant burden of premature mortality.

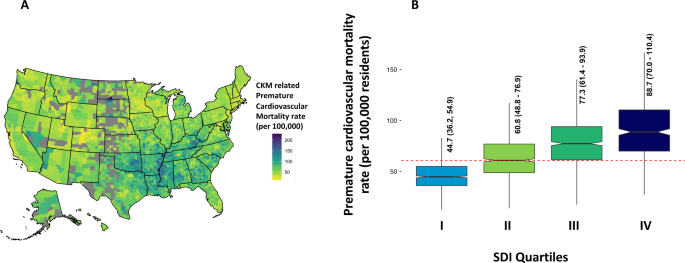
The study, conducted by a team of researchers, analyzed state-level and county-level data on CKM-associated premature cardiovascular mortality (defined as death before age 65) across the United States from 2010 to 2019. They then linked this data to the Social Deprivation Index (SDI), a comprehensive metric that captures various socioeconomic factors, such as poverty, education, employment, housing, and access to resources.
Stark Disparities Across the US
The findings were striking. The researchers found that the median CKM-related premature cardiovascular mortality rate in the US was 60.7 per 100,000 residents. However, this rate varied significantly across different regions and socioeconomic groups.
Geographic Differences: Mississippi and Oklahoma had the highest CKM-related premature mortality rates, while Minnesota reported the lowest. These geographic disparities were further exacerbated by the level of social deprivation in each county.
Socioeconomic Disparities: As the social deprivation index (SDI) increased, so did the CKM-related premature mortality rates. Counties in the highest SDI quartile (most deprived) had a 40% higher mortality rate compared to the national average.
Disproportionate Burden on Vulnerable Populations
The study also uncovered significant disparities within the population. Men had higher CKM-related premature mortality rates than women, and non-Hispanic Black residents had nearly double the rates of non-Hispanic White residents. Furthermore, residents of rural and non-metropolitan counties faced a higher burden of CKM-related premature mortality compared to their urban counterparts.
Gender Differences: The median CKM-related premature mortality rate for men was 84.9 per 100,000 residents, compared to 40.7 per 100,000 for women.
Racial Disparities: Non-Hispanic Black residents had a median CKM-related premature mortality rate of 110.1 per 100,000, while non-Hispanic White residents had a rate of 58.8 per 100,000.
Urban-Rural Divide: Non-metropolitan counties had a median CKM-related premature mortality rate of 66.3 per 100,000, compared to 54.3 per 100,000 in metropolitan counties.
Addressing the Root Causes
The study’s findings highlight the urgent need to address the underlying social determinants of health that contribute to these disparities. Factors such as poverty, lack of access to education and healthcare, and poor living conditions can all have a significant impact on an individual’s cardiovascular health and risk of premature mortality.
