
Psoriatic arthritis is a chronic inflammatory condition that affects the joints, tendons, and entheses, often leading to progressive joint damage and disability. In recent years, the treatment landscape for psoriatic arthritis has expanded with the introduction of various biological disease-modifying anti-rheumatic drugs (bDMARDs) targeting different mechanisms of action. This has led to an important clinical question – which switching strategy works best when the first bDMARD fails? A new real-world study has investigated this, comparing the effectiveness of cycling between tumor necrosis factor alpha (TNF-α) inhibitors versus swapping from TNF-α inhibitors to interleukin-17 (IL-17) inhibitors, or vice versa. The findings suggest that in clinical practice, swapping from TNF-α inhibitors to IL-17 inhibitors may be more effective than cycling between TNF-α inhibitors. This study provides valuable insights into optimizing treatment strategies for patients with psoriatic arthritis. Psoriatic arthritis, Biological disease-modifying anti-rheumatic drugs, Tumor necrosis factor, Interleukin-17
Understanding Psoriatic Arthritis and its Treatment
Psoriatic arthritis is a chronic, inflammatory autoimmune condition that affects the joints, tendons, and entheses (the areas where tendons and ligaments attach to bones). This condition can lead to progressive joint damage and functional disability if left untreated. In recent years, the treatment options for psoriatic arthritis have expanded significantly with the introduction of various biological disease-modifying anti-rheumatic drugs (bDMARDs) that target different mechanisms of action.
The first bDMARDs available for psoriatic arthritis were the tumor necrosis factor alpha (TNF-α) inhibitors, such as infliximab, etanercept, adalimumab, golimumab, and certolizumab pegol. Subsequently, interleukin (IL)-17 inhibitors, such as secukinumab, ixekizumab, and bimekizumab, as well as inhibitors of IL-12/23, IL-23, cytotoxic T-lymphocyte antigen 4, phosphodiesterase-4, and Janus kinase, have been introduced, expanding the number of therapeutic options for patients.
Exploring Treatment Switching Strategies
While the current guidelines recommend starting with TNF-α inhibitors for the treatment of psoriatic arthritis, there is no clear consensus on the best strategy to follow when the first bDMARD fails. In clinical practice, the two most common switching scenarios are:
1. Cycling: Switching from one TNF-α inhibitor to another TNF-α inhibitor.
2. Swapping: Switching from a TNF-α inhibitor to an IL-17 inhibitor, or vice versa.
Preliminary observational studies have suggested that the swapping strategy may be slightly more effective than cycling, but the evidence has been inconclusive. This real-world study aimed to provide a more comprehensive understanding of the effectiveness of these two switching strategies in clinical practice.
Investigating Cycling vs. Swapping Strategies
The researchers conducted a single-center, retrospective, observational study involving 122 patients with psoriatic arthritis who were treated with TNF-α inhibitors and/or IL-17 inhibitors between January 2016 and January 2022. The patients were divided into three subgroups based on their switching strategy:
1. Cycling Group (CG): Patients who switched from one TNF-α inhibitor to another TNF-α inhibitor.
2. Swap Group 1 (SG1): Patients who switched from a TNF-α inhibitor to an IL-17 inhibitor.
3. Swap Group 2 (SG2): Patients who switched from an IL-17 inhibitor to a TNF-α inhibitor.
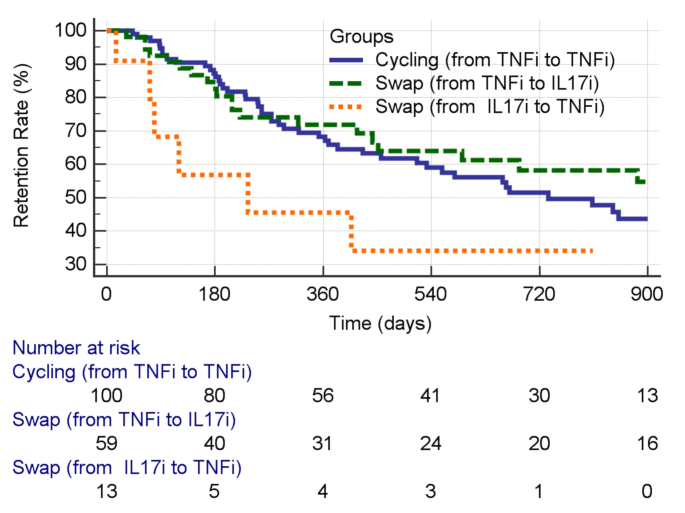
The researchers then compared the effectiveness of these strategies, measured by the drug retention rate (the time a patient remained on the prescribed treatment).
Findings and Implications
The results of this study suggest that in real-world clinical practice, the swapping strategy from TNF-α inhibitors to IL-17 inhibitors (SG1) may be more effective than cycling between TNF-α inhibitors (CG). The 2-year retention rate was 58% in SG1, compared to 51% in CG and 34% in SG2.
The researchers also identified several factors that influenced the retention rate:
1. Swapping from TNF-α inhibitors to IL-17 inhibitors was associated with a longer treatment persistence.
2. Younger age and lower disease activity at baseline were also linked to better treatment persistence.
3. The year of the switch also affected the retention rate, likely due to changes in treatment strategies or the availability of new therapeutic options over time.
These findings have important implications for the management of psoriatic arthritis in clinical practice. The study suggests that when the first bDMARD fails, swapping to an IL-17 inhibitor may be a more effective strategy than cycling between TNF-α inhibitors. This information can help clinicians make more informed decisions when selecting the optimal treatment pathway for their patients.
Limitations and Future Research
It’s important to note that this study has limitations, as it was a retrospective, observational study conducted at a single center. The researchers acknowledged potential biases, such as the selection of patients, the influence of patient characteristics on the choice of treatment strategy, and the low number of patients in the SG2 subgroup (swapping from IL-17 inhibitors to TNF-α inhibitors).
Despite these limitations, this study provides valuable insights into the real-world management of psoriatic arthritis and highlights the need for further research to confirm the findings and explore the underlying mechanisms that may explain the potential advantages of the swapping strategy. Larger, multicenter studies with longer follow-up periods would help to validate these results and provide a more comprehensive understanding of the optimal treatment sequencing for patients with psoriatic arthritis.
Author credit: This article is based on research by Federica Lumetti, Alarico Ariani, Antonio Marchesoni, Andrea Becciolini, Dilia Giuggioli, Gilda Sandri.
For More Related Articles Click Here
