Check out innovative research that has merged exosomes with hydrogels to create a novel way of healing wounds related to diabetes — ideally leading to improvements in healing and decreasing the secondary complications.
Extracellular Vesicles: Nature’s Tiny MolecularHealers
Millions across the globe are living with diabetes, with wound healing among its most devastating complications. Historically, traditional therapies have been ill-suited to confront the special challenges of diabetic wounds, which include inhibited oxygen levels and diminished blood vessel growth.
A new area of biomedical research, however, is providing a bit of optimism. Scientists at NYU Langone and NYU Tandon, led by Jin Kim Montclare, have been studying the promise of exosomes — miniscule lipid-bilayered vesicles loaded with a plethora of biological contents such as nucleic acids, proteins, and lipids. To that end, nanovesicles have an incredible capacity for helping cells to communicate with one another and regulate everything from tissue repair to inflammation control.
Exosomes secreted from human adipose-derived mesenchymal stem cells (ASC) have been implicated as potential regulators of wound healing based on ex-vivo and animal studies. Their therapeutic benefits are believed to be due in part to their anti-inflammatory properties and by promoting a pro-healing environment, which includes increased blood vessel formation, as well as transmission of key cells such as fibroblasts and endothelial cells into the defect.
Hydrogels: the Source to Bridge the Gap
And while exosomes show promise, one challenge researchers face is that they must be administered multiple times — typically by a distracting or intravenous injection — which can complicate long-term wound care. To solve this problem, Montclare and her team have been investigating creative methods to boost the therapeutic effects of exosomes, with a particular advance being their combination with hydrogels.
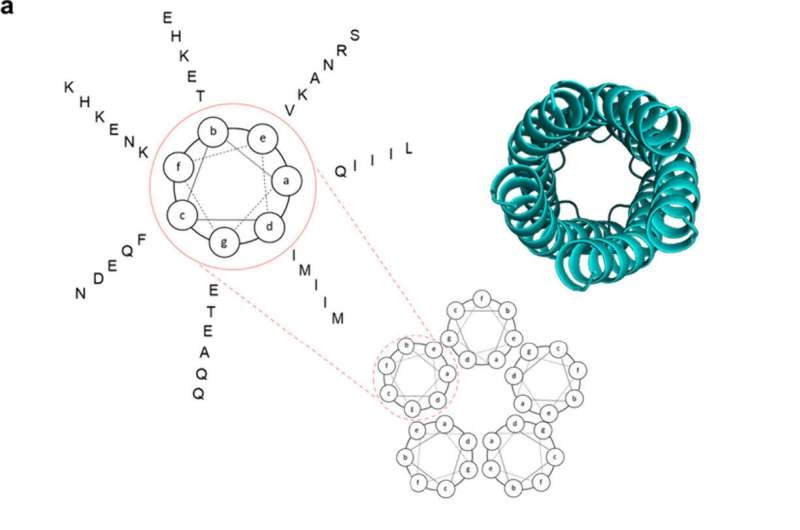
Hydrogels are networks of cross-linked polymers that can be used to encapsulate exosomes. This packaging could offer a more prolonged and localized release of exosomes at the wound site rather than having to inject invasive treatments. Since hydrogels are biocompatible and able to keep wounds hydrated, they function fine as wound dressings in their own right.
The application of these hydrogel systems, especially for diabetic wounds, is greatly improved by combining them with exosomes. In a more recent study, combinations of exosomes with hydrogels have been consistently shown to be able to cause faster wound closure than the individual usage of either hydrogel or exosome. By demonstrating the effective acceleration of diabetic wound healing with exosome-loaded hydrogels, we present an innovative approach to a potential new generation of biocompatible, high-yield wound dressing scaffolds in catelling exosomes for the revolutionizing of diabetic wound treatment.
Conclusion
First ever combined use of exosomes and hydrogels like featured to treat diabetic wounds: This novel research has opened the gateway for promising prospects in the treatment of diabetic wounds. Scientists have harnessed the wound-healing benefits of exosomes and the unique properties of hydrogels to create an exciting new avenue for advancing wound-healing outcomes in diabetes, with potential clinical use on the horizon. In the years to come, this area of research will only continue and we can look forward to increasingly creative developments for diabetic wound care solutions.
