Researchers at the University of Michigan have developed a new microchip that can detect lung cancer from a simple blood draw, making the process 10 times faster and 14 times more sensitive than previous methods. The chip captures exosomes, tiny packages released by cells, which contain valuable information about cancer. This technology holds great promise for improving early detection and treatment of lung cancer. Lung cancer is one of the most deadly forms of cancer, and early detection is critical for effective treatment.
Solving the Riddle of Why Lung Cancer can be Diagnosed Early
Historically, lung cancer has been challenging to detect in its early stages which has resulted in late-stage diagnoses and poorer survival prospects for patients. University of Michigan scientists have developed a new microchip that offers an alternative solution to the manufacturing and infrastructure problem.
The chip collects exosomes–minuscule vesicles that are shed by cells, including cancer cells. The exosomes carry with them proteins and genetic material that indicate the presence of lung cancer. With a focus on these exosomes, the researchers came up with an assay capable of producing results in about 10 hours and showing about 14 times more sensitivity than previous blood-based diagnostic techniques.
The study’s co-corresponding author Sunitha Nagrath, a U-M professor of chemical and biomedical engineering; said cancer exosomes that escape the tumor microenvironment would “go out and sort of till the soil. A few years later, the cancer cell seeds disperse from the tumor”s plant to lead a lavish and lovely life in conditioned soil as they travel through the bloodstream to get planted and began flourishing. As such, the microchip could diagnose lung cancer earlier than a typical tumor would materialize by detecting whether these signaling exosomes are present.
The Microchip Science
What makes the chip special is its ability to sense much of what distinguishes cancer-related exosomes from those that come from healthy cells. The proteins on the surface of these minuscule bags are prone to mutations that alter the way they look and how they interact with light.
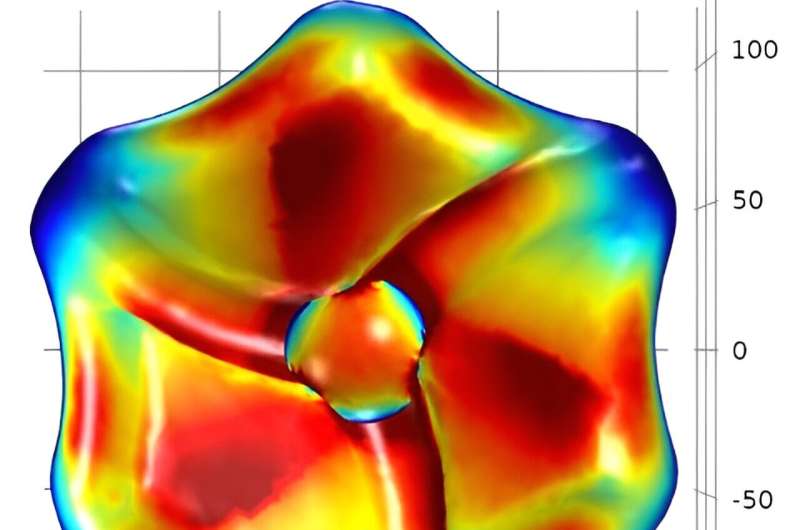
In this case, the researchers created a right-twisting gold nanoparticle to grab exosomes in its central cavity. This area, which is focused on the exosomes, replicates presumably corresponding dimensions and shape of this cavity or alternatively to reliably capture particles. The exosomes bound to them in turn exert the same force on a twisted light, producing a unique signal that researchers can detect and study.
“I thought that these nanoparticles would be sensitive to the mutations in proteins because they present an optical activity but was surprised how great this sensitivity turned out to be,” said Nicholas Kotov, the Irving Langmuir Distinguished University Professor of Chemical Sciences and Engineering at U-M and co-corresponding author on the study. The reason is that all the particles are in alignment in detection tool.
Supplemental CT: The Future of Lung Cancer Screening?
The researchers see the CDEXO chip, as they’ve (somewhat tortuously) dubbed it will first be utilized to work local conventional analysis strategies, so that individuals can develop rely on and religion within the technology. If the chip also demonstrates comparable accuracy and reliability, then it eventually could be run as a stand-alone test for lung cancer and possibly other types of cancer.
For the next steps, we will explore the differences in their spectral signatures for most known solid tumor mutated proteins. This is about as far as we can push the technology to maximise those spectral differences and discriminate one protein from another,” added Nagrath.
This breakthrough in lung cancer screens is likely to save millions of lives in the future. The CDEXO chip is therefore a potentially powerful new approach to diagnose PAD at its earliest stages, so that patients can receive earlier interventions and tailored therapies leading to better outcomes. The research team is still making improvements and building out the feature set, but if they are successful, this could be a bright light for how we diagnose cancer in the future.
