Ceftriaxone, a powerful antibiotic, has become a cornerstone of global healthcare, but its widespread misuse is fueling the alarming rise of antimicrobial resistance. A recent systematic review and meta-analysis by researchers in Ethiopia has shed light on this critical issue, revealing that over half of ceftriaxone usage in the country is inappropriate. This concerning finding underscores the urgent need for targeted interventions to promote the rational use of this vital drug and safeguard its effectiveness for the future. Ceftriaxone, a third-generation cephalosporin, is a widely prescribed antibiotic known for its potent antibacterial activity, broad spectrum coverage, and low toxicity. However, the study highlights how its misuse, through practices like overuse, improper dosing, and deviation from established guidelines, is jeopardizing its efficacy and contributing to the global crisis of antimicrobial resistance. The findings emphasize the pressing need for improved antibiotic stewardship, enhanced clinician education, and the adoption of rapid diagnostic tools to ensure the appropriate use of ceftriaxone and safeguard this critical resource for future generations.
Ceftriaxone: A Double-Edged Sword
Ceftriaxone is a widely used antibiotic that has become a cornerstone of modern medicine, offering a potent and versatile weapon against a wide range of bacterial infections. However, this very strength has also made it a prime target for misuse, with the study revealing that an alarming 55.24% of ceftriaxone usage in Ethiopia is inappropriate. This concerning trend is not unique to Ethiopia, as similar issues have been reported in other parts of the world, underscoring the global nature of this challenge.
Uncovering the Drivers of Ceftriaxone Misuse
The researchers delved deep into the factors contributing to the inappropriate use of ceftriaxone in Ethiopia. One of the key drivers identified was the heavy reliance on empiric therapy, where treatment is initiated without confirming the diagnosis through laboratory tests. This practice, often driven by limited access to diagnostic capabilities, can lead to the indiscriminate use of broad-spectrum antibiotics like ceftriaxone, even when a narrower, more targeted approach may be more appropriate.
Another significant factor was the co-prescription of multiple medications, which was found to increase the likelihood of ceftriaxone being used inappropriately. Additionally, the study highlighted that certain hospital departments, particularly the emergency and surgery wards, exhibited higher rates of non-compliance with established guidelines for ceftriaxone use.
Addressing the Threat of Antimicrobial Resistance
The overuse and misuse of ceftriaxone, as revealed in this study, pose a serious threat to public health. Inappropriate antibiotic usage is a primary driver of the antimicrobial resistance crisis, which has the potential to render once-treatable infections untreatable, leading to increased morbidity, mortality, and healthcare costs.

Table 1 Descriptive summary of the 17 included studies in the meta-analysis of Ceftriaxone drug utilization pattern, Ethiopia.
To combat this challenge, the researchers emphasize the urgent need for a multifaceted approach, including:
1. Improved Antibiotic Stewardship: Implementing robust antibiotic stewardship programs that promote the judicious use of ceftriaxone and other antibiotics, ensuring adherence to established guidelines and reducing unnecessary prescriptions.
2. Enhanced Clinician Education: Providing comprehensive training and resources for healthcare professionals to improve their understanding of appropriate antibiotic usage, resistance patterns, and the importance of adherence to treatment protocols.
3. Adoption of Rapid Diagnostic Tools: Investing in the development and deployment of rapid diagnostic tests that can quickly identify the causative agents of infections, enabling healthcare providers to prescribe targeted, narrow-spectrum antibiotics instead of relying on broad-spectrum options like ceftriaxone.

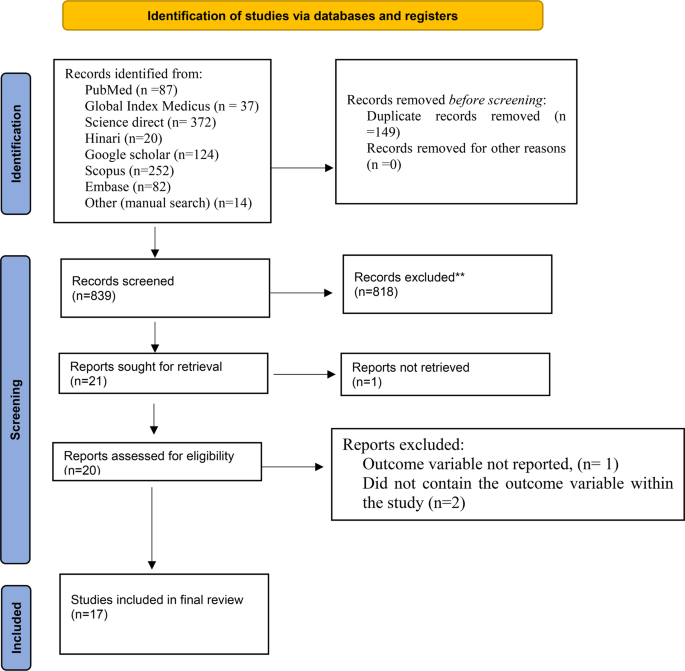
Fig. 2
Broader Implications and Future Directions
The findings of this study have far-reaching implications, not just for Ethiopia, but for the global healthcare community. The high prevalence of inappropriate ceftriaxone use observed in this research mirrors similar challenges faced by other developing nations, underscoring the need for coordinated, international efforts to address this issue.
Beyond the immediate concerns, this study also highlights the importance of continued research and collaboration in the field of antimicrobial resistance. By expanding our understanding of the drivers and patterns of antibiotic misuse, researchers can inform the development of more effective interventions and policies to safeguard the long-term effectiveness of these vital drugs. As we navigate the complex landscape of antimicrobial resistance, studies like this one serve as a critical guide, empowering healthcare providers, policymakers, and the public to take decisive action in preserving the efficacy of ceftriaxone and other antibiotics for generations to come.
Author credit: This article is based on research by Chernet Tafere, Destaw Endeshaw, Desalegn Getnet Demsie, Malede Berihun Yismaw, Bereket Bahiru Tefera, Adane Yehualaw, Kebede Feyisa, Ebrahim Abdela Siraj, Ashagrachew Tewabe Yayehrad, Zenaw Debasu Addisu, Ousman Adal.
For More Related Articles Click Here
