Diabetes is a major risk factor for developing heart failure, a serious condition where the heart struggles to pump blood effectively. Researchers have now uncovered a promising new treatment approach that could revolutionize the management of this debilitating complication. Their study, published in the journal Scientific Reports, shows how a drug called sacubitril/valsartan (Sac/Val) can dramatically improve the stiffness of the heart’s left ventricle in diabetic mice, a key driver of diastolic dysfunction and heart failure with preserved ejection fraction (HFpEF). This groundbreaking discovery sheds light on the underlying mechanisms and opens up new avenues for treating this challenging form of heart disease.
Unraveling the Complexities of Diabetic Heart Failure
Heart failure is a devastating condition that affects millions worldwide, and its prevalence is only expected to rise as the global diabetes epidemic continues. Approximately half of all heart failure patients have a preserved ejection fraction, meaning their heart’s ability to pump blood remains relatively normal. However, these individuals often struggle with impaired diastolic function, where the heart’s relaxation and filling are compromised, leading to symptoms like shortness of breath, fatigue, and edema.
Diabetes is a major contributor to the development of this type of heart failure, known as HFpEF. The metabolic disturbances associated with the disease can cause structural and functional changes in the heart, including increased stiffness of the left ventricle. This stiffening makes it harder for the heart to fill with blood during diastole, the relaxation phase of the cardiac cycle, ultimately impairing its ability to pump effectively.
Uncovering the Molecular Mechanisms
In the current study, the researchers used a mouse model of type 1 diabetes to investigate the effects of sacubitril/valsartan, a combination drug that inhibits the breakdown of beneficial natriuretic peptides. These peptides activate the kinaseG’>PKG signaling pathway, which has been shown to play a crucial role in regulating the stiffness of the heart’s main pumping chamber, the left ventricle.
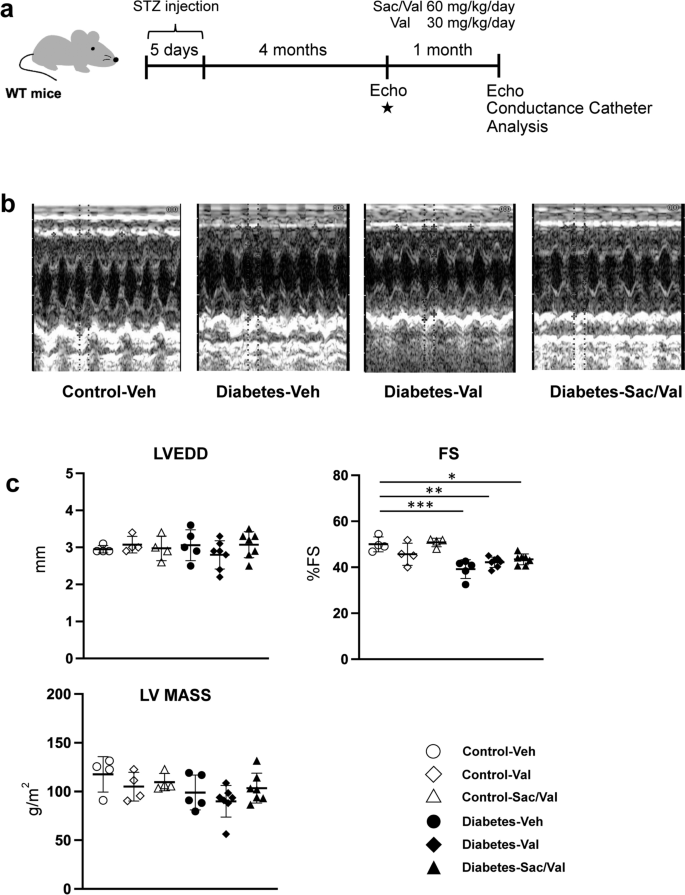
The researchers found that Sac/Val treatment significantly reduced the increased left ventricular stiffness observed in the diabetic mice, compared to those receiving the individual component, valsartan, or a control treatment. Importantly, this improvement in diastolic function was not accompanied by changes in cardiac fibrosis or the expression of key calcium-handling proteins, suggesting that the beneficial effects of Sac/Val were primarily mediated through modifications to the giant sarcomeric protein, titin.
Titin acts as a molecular spring within the heart’s muscle fibers, and its phosphorylation state is a major determinant of passive ventricular stiffness. The researchers demonstrated that Sac/Val treatment led to a greater increase in the phosphorylation of the N2B region of titin, which is known to be associated with reduced stiffness, compared to valsartan alone.

Further analysis revealed that Sac/Val enhanced the activation of the cGMP-PKG signaling pathway to a greater extent than valsartan, providing a mechanistic explanation for the observed improvements in diastolic function. This suggests that the inhibition of natriuretic peptide degradation by sacubitril, the neprilysin inhibitor component of the drug, plays a key role in mediating these beneficial effects.
Implications and Future Directions
The findings of this study have important implications for the management of diabetic heart failure, particularly the HFpEF subtype. By targeting the underlying molecular mechanisms that contribute to ventricular stiffening, Sac/Val offers a promising therapeutic approach to improve diastolic function and potentially alleviate the debilitating symptoms experienced by patients.
Moreover, the insights gained into the role of titin phosphorylation and cGMP-PKG signaling in regulating cardiac stiffness open up new avenues for further research and drug development. Exploring strategies to directly modulate titin properties or enhance the cGMP-PKG pathway may yield additional therapeutic options for this challenging form of heart failure.
Broader Implications and Future Directions
The findings of this study not only have implications for the treatment of diabetic heart failure but also contribute to our broader understanding of the mechanisms underlying cardiac dysfunction in various disease states. The pivotal role of titin and its post-translational modifications in determining ventricular stiffness has been a subject of increasing interest in the field of cardiovascular research.
Beyond diabetes, the insights gained from this study may inform the development of therapies for other conditions associated with diastolic dysfunction, such as hypertension, aging, and certain genetic cardiomyopathies. Furthermore, the use of advanced techniques like mass spectrometry to map the specific phosphorylation sites on titin could lead to the identification of novel therapeutic targets and the design of more targeted interventions.
As the scientific community continues to unravel the complex interplay between metabolic disorders, cardiac structure, and function, studies like this one hold the promise of revolutionizing the way we approach the management of heart failure, ultimately improving the quality of life for millions of patients worldwide.
Meta description: Researchers uncover how a breakthrough drug, sacubitril/valsartan, can dramatically improve cardiac function in diabetic heart failure by targeting the giant protein titin and enhancing cGMP-PKG signaling.
For More Related Articles Click Here
