As the COVID-19 pandemic continues to impact communities worldwide, researchers have been investigating the role of common hypertension medications in influencing the course of the disease. A recent study published in the journal Scientific Reports has shed light on the distinct effects of two widely prescribed antihypertensive drugs, losartan and enalapril maleate, on SARS-CoV-2 infection in Vero E6 cells. The findings hold significant implications for understanding the complex interplay between COVID-19, the renin-angiotensin system, and potential therapeutic strategies.

Hypertension Drugs and COVID-19: A Complex Relationship
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has posed unprecedented challenges to global healthcare systems. Individuals with pre-existing conditions, such as hypertension, have been identified as particularly vulnerable to severe COVID-19 outcomes. This has raised concerns about the potential impact of commonly prescribed antihypertensive medications on the progression of the disease.
Investigating the Effects of Losartan and Enalapril Maleate
In this study, researchers from the Pontifical Catholic University of Rio Grande do Sul in Brazil set out to examine the influence of two widely used antihypertensive drugs, losartan and enalapril maleate, on SARS-CoV-2-infected Vero E6 cells, a common model for studying the virus.
The researchers first assessed the cytotoxicity of these medications on Vero E6 cells, finding that both drugs were well-tolerated, with cell viability levels exceeding 80% even at the highest concentrations tested.

Fig. 2
Distinct Antiviral Effects of Losartan and Enalapril Maleate
The study then focused on evaluating the antiviral activity of these medications. The results revealed a remarkable difference between the two drugs. Losartan treatment significantly reduced the levels of SARS-CoV-2 nucleocapsid RNA to near-undetectable levels, indicating a potent inhibitory effect on viral replication. In contrast, enalapril maleate did not demonstrate a significant impact on viral RNA levels.
These findings suggest that losartan, an angiotensin II receptor blocker (ARB), may interfere with SARS-CoV-2 infection and replication through mechanisms that are distinct from the angiotensin-converting enzyme inhibitor (ACEi) enalapril maleate.

Fig. 3
Modulation of Cellular Pathways and Biomarkers
The researchers also investigated the impact of these medications on the expression of various genes and cellular pathways related to the host’s response to SARS-CoV-2 infection. The analyses revealed distinct profiles of gene expression between infected cells treated with losartan or enalapril maleate.
For instance, infected cells treated with losartan showed no significant changes in the expression of interleukin-6 (IL-6) compared to infected-untreated cells. In contrast, infected cells treated with enalapril maleate exhibited higher IL-6 mRNA levels, suggesting a potential pro-inflammatory effect of this ACEi.
Furthermore, the study found that infected cells treated with enalapril maleate showed increased expression of p53, p21, and p62, indicating the involvement of these cellular pathways in the host’s response to SARS-CoV-2 infection. These findings highlight the complex interplay between antihypertensive medications, viral infection, and the modulation of cellular signaling cascades.
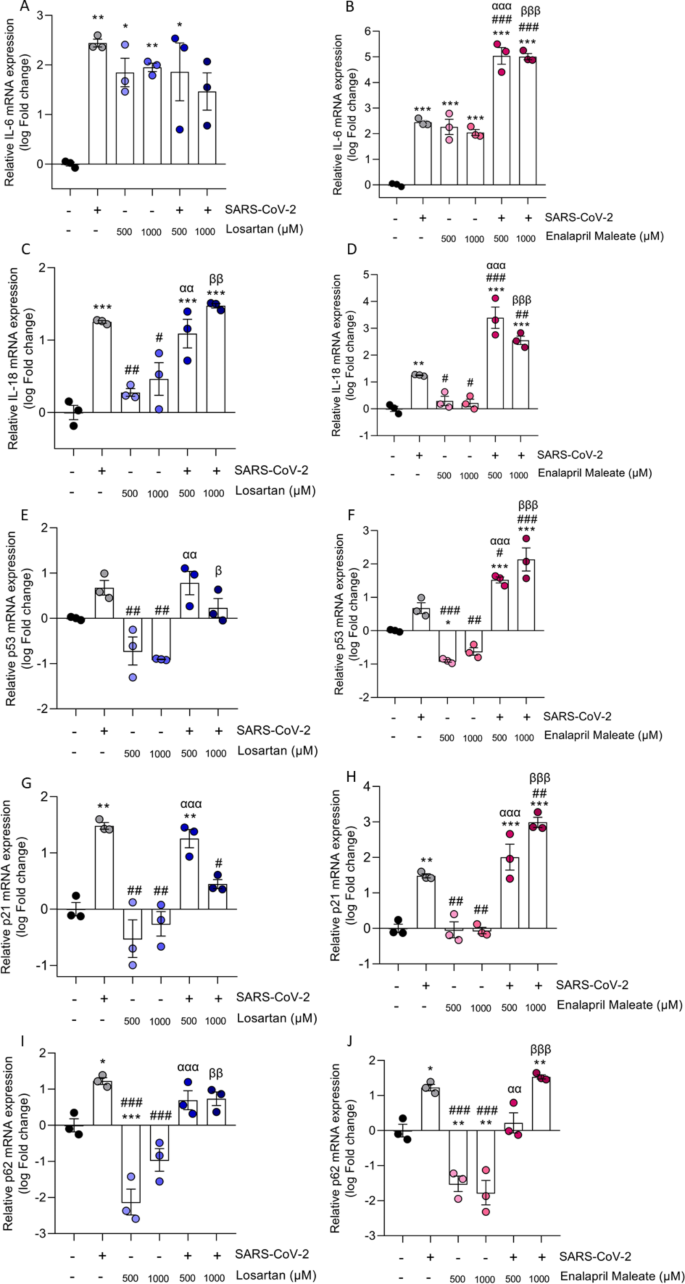
Fig. 4
Implications and Future Directions
The data from this study suggest that losartan and enalapril maleate can differentially influence the effects triggered by SARS-CoV-2 infection in Vero E6 cells. While losartan appears to significantly reduce viral replication, enalapril maleate does not demonstrate the same antiviral efficacy. These findings have important implications for understanding the potential therapeutic applications of these medications in the context of COVID-19.
The study’s insights also highlight the need for further research to elucidate the precise mechanisms by which these antihypertensive drugs modulate the host’s response to SARS-CoV-2 infection. Exploring the impact on various cell types, clinical outcomes, and potential synergistic effects with other therapies could provide valuable insights for developing more effective COVID-19 treatment strategies.
As the scientific community continues to unravel the complexities of the COVID-19 pandemic, studies like this one contribute to our understanding of the intricate relationship between pre-existing conditions, medication use, and the body’s response to SARS-CoV-2 infection. These findings may pave the way for more personalized and targeted approaches in managing COVID-19, particularly for individuals with hypertension.
Author credit: This article is based on research by Julia H. Majolo, João I. B. Gonçalves, Renata P. Souza, Laura C. González, Nathalia Sperotto, Maiele D. Silveira, Sílvia D. Oliveira, Cristiano V. Bizarro, Pablo Machado, Luiz A. Basso, Ana P. D. Souza, Jarbas R. Oliveira, Carlos A. S. Ferreira.
For More Related Articles Click Here
