Researchers have developed a powerful predictive model that combines advanced ultrasound imaging techniques and clinical data to accurately distinguish between benign and malignant liver lesions. This non-invasive approach outperforms current diagnostic methods, offering a promising tool for early and precise detection of liver cancer. The model leverages the unique capabilities of Sonazoid contrast-enhanced ultrasound and Sound Touch Elastography, providing invaluable insights into tumor blood flow and tissue stiffness. With its exceptional accuracy, this innovative ultrasound-based model has the potential to transform the way liver cancer is diagnosed and managed, leading to better patient outcomes.

Main content:
Unlocking the Secrets of Liver Lesions
Liver cancer is a complex and challenging disease, with accurate diagnosis often crucial for determining the best course of treatment. Traditional imaging techniques, such as conventional ultrasound, have faced limitations in reliably distinguishing between benign and malignant liver lesions. However, a team of researchers has developed a groundbreaking predictive model that combines the power of advanced ultrasound imaging and clinical data, revolutionizing the way liver cancer is detected.
The Fusion of Cutting-Edge Ultrasound Technologies
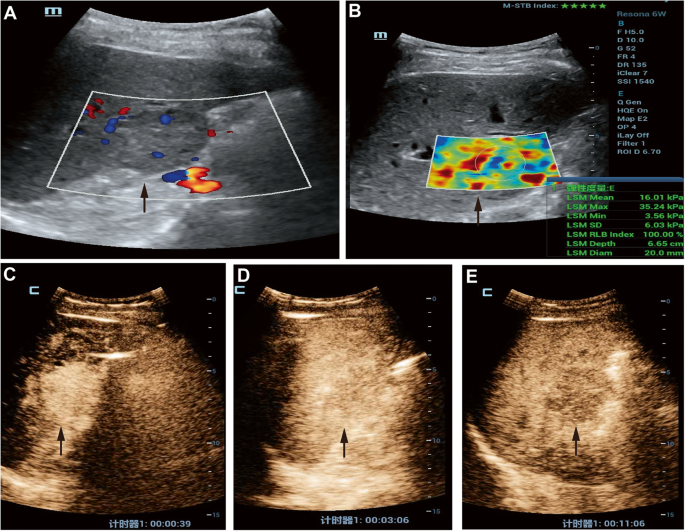
The key to this innovative approach lies in the integration of two cutting-edge ultrasound techniques: Sonazoid contrast-enhanced ultrasound (SCEUS) and Sound Touch Elastography (STE). SCEUS, a liver-specific contrast agent, provides unparalleled insights into the tumor’s blood flow patterns, while STE measures the tissue’s elasticity, or stiffness, which can be a reliable indicator of malignancy.
Unleashing the Predictive Power
The researchers developed a sophisticated predictive nomogram model that combines the image features from SCEUS and STE, along with relevant clinical data, to accurately differentiate between benign and malignant liver lesions. This multi-modal approach allows for a comprehensive evaluation of the lesions, reducing the risk of missed diagnoses or misclassifications.
Outperforming Current Diagnostic Methods
The study demonstrated the remarkable performance of this ultrasound-based predictive model, with an area under the receiver operating characteristic (AUC) curve of 0.988 and 0.978 in the training and test sets, respectively. This significantly outperformed the diagnostic accuracy of the widely used CEUS Liver Imaging Reporting and Data System (CEUS LI-RADS) and STE alone.
Improving Clinical Decision-Making
The integration of SCEUS, STE, and clinical features into the predictive model provides a powerful tool for clinicians to make informed decisions about the nature of liver lesions. By accurately distinguishing benign from malignant lesions, this non-invasive approach can help guide the selection of appropriate treatment strategies, ultimately leading to better patient outcomes.
Paving the Way for Personalized Liver Cancer Care
The researchers emphasize the potential of this ultrasound-based predictive model to revolutionize the way liver cancer is diagnosed and managed. By offering a reliable, non-invasive, and highly accurate method, the model holds the promise of enabling early and precise detection of malignant lesions, empowering clinicians to tailor personalized treatment plans for their patients.
As the scientific community continues to explore the frontiers of medical imaging and data-driven diagnostics, this innovative ultrasound-based predictive model stands as a shining example of how advancements in technology can profoundly impact the way we approach complex healthcare challenges.
Author credit: This article is based on research by Qianqian Shen, Wei Wu, Ruining Wang, Jiaqi Zhang, Liping Liu.
For More Related Articles Click Here
