Researchers have made a breakthrough in understanding the genetic basis of type I CD36 deficiency, a rare condition where the body lacks a crucial protein called CD36. Using advanced DNA sequencing techniques, the study identified key genetic variants and haplotypes (a collection of genetic variants inherited together) that contribute to this deficiency. The findings shed light on how mutations in the CD36 gene, particularly in the gene’s regulatory regions, can disrupt the production of the CD36 protein and lead to the type I form of the deficiency. This discovery could pave the way for improved diagnosis, monitoring, and potentially even targeted therapies for individuals with this condition. CD36 is a protein that plays a crucial role in various cellular processes, and understanding its genetic underpinnings is crucial for advancing our knowledge of human health and disease.
Unraveling the Genetic Basis of CD36 Deficiency
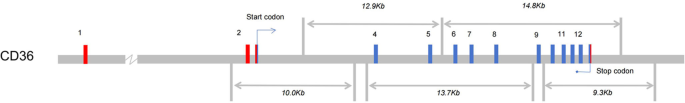
CD36, also known as glycoprotein IV, is a membrane protein expressed on various cell types, including monocytes, platelets, and endothelial cells. It plays a vital role in a wide range of cellular processes, from fatty acid metabolism to immune function. However, some individuals may lack the expression of CD36, a condition known as CD36 deficiency.
There are two main types of CD36 deficiency: type I, where the protein is completely absent, and type II, where it is absent on platelets but present on monocytes. Individuals with type I deficiency are generally healthy but may develop antibodies against CD36 after blood transfusions or during pregnancy, leading to complications such as Click Here
